For nearly a century, we humans have depended on our secret weapon for cure of many otherwise lethal bacterial infections. Antibiotics, which are naturally produced by bacteria and fungi, are now available to treat countless infections and illnesses associated with harmful bacteria. It’s safe to say that natural and synthetic antibiotics save more lives than Batman ever could. So, you may be wondering, “what’s the issue”? The issue isn’t the antibiotics themselves, it is resistance to them that could potentially diminish all antibiotic effectiveness as we know it.
What Is Antibiotic Resistance?
Antibiotic resistance is a fairly simple concept. Antibiotic resistance, or not being impacted by the antibiotic, can be innate or acquired. Innate means the bacteria naturally have some sort of structural or chemical property that inhibits the action of a certain antibiotic. Antibiotics are used to kill harmful bacteria, and they generally do so very well (if the proper antibiotic is given). Sometimes, however, some of the bacteria the antibiotic is acting against is resistant to the drug. When the few resistant ones survive while the others die, these ones remain and multiply or horizontally transferring their resistant genes (aka conjugation) to others nearby. Thus, a whole village of bacteria resistant to that antibiotic is created. This, and the spontaneous mutation that can randomly occur in bacterial genes, are called acquired resistance. According to a recent BBC article, overprescribing, casually prescribing, and improper use of antibiotics, are all things that can lead to a bacteria strain becoming an incurable superbug.
Resistance is actually a really scary thing. According to the BBC article, there has been a 35% increase in antibiotic-resistant blood infections in England. Over the past four years, England’s cases of sepsis, or bacteria in the blood, have increasingly become harder to treat due to resistance. While this article discusses the UK, the same issue is present in the United States and many other medically-advanced nations. Perhaps if more studies were conducted on alternative treatments or procedures for some bacterial illnesses, we could mitigate antibiotic resistance. If we continue at the rate we’re going, we may never be able to use antibiotics for treatment of deadly infections. The Center for Disease Control, luckily, is advocating for this awareness.
Resistant Organisms
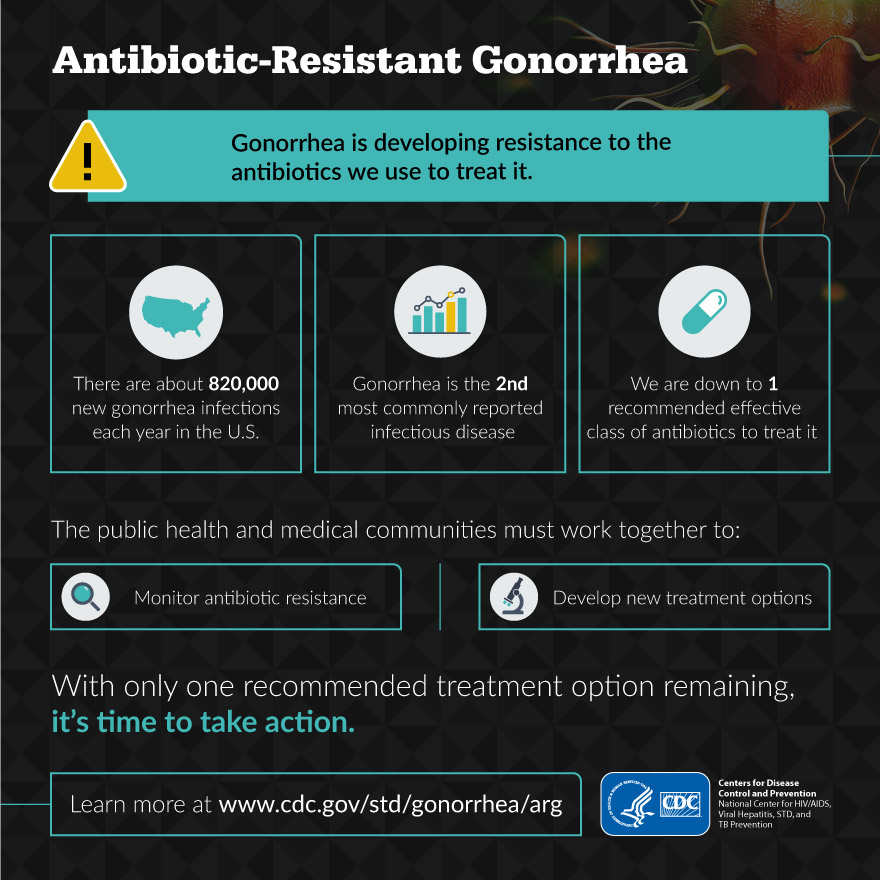
One known resistant organism that is increasing becoming a red flag in the medical community is Neissera gonorrhoeae. This is what causes the ever-so-feared STD, gonorrhea. According to the CDC, more strains of gonorrhea have increasingly developed a resistance to nearly every drug used to treat it, including Cephalosporin. According to a CDC video, many cases of gonorrhea do not cause symptoms but the consequences of having it can still be life-threatening. Resistance in N. gonorrhoeae is thought to be acquired rather than innate, then continuously spread. But don’t panic just yet– there’s still hope. Antibiotic treatment is still available, although not in variety. I think Neissera gonorrhoeae is one of the best case scenario of an antibiotic-resistant organism because of how easily it can be refrained from spreading. It is important to use proper protection and know your sexual partner’s STI history, if any. Stay safe, kids.
In contrast to N. gonorrhoeae, some organisms are resistant because of their genetic makeup. In the case of CREs, their family lineage grants them drug resistance. Isn’t that great.
A Carbapenem-resistant Enterobacteriaceae (CRE) is a gram-negative bacterium in the Enterobacteriaceae family, including species of Klebsiella, E.coli, and salmonella. According to the CDC, CREs are known to be very resistant to Carbapenem, a strong drug typically used as the “last resort” for a variety of bacterial infections. CREs are resistant as they produce carbapenemases (i.e, klebsiella pneumoniae carbapenemase) that break down the antibiotic. The same article also mentions how CRE infections are healthcare-related, which basically means they tend to occur due to extensive hospital treatments. Salmonella enterica is a common CRE threat. According to a Health article, there was an outbreak of Salmonella last year by a highly resistant and virulence strain of S.enterica. This strain sickened nearly 92 people nationwide and is resistant to 12 different antibiotics. As we learned in class, Salmonella typically goes away without antibiotic treatment; I’m curious to know if these resistant strains would be able to do that, or if they are too virulent to be left alone. In this case, treatment was mainly achieved through combination therapy.
Salmonella is transmitted through contaminated poultry to humans. In contrast, Gonorrhea is transmitted from human to human. Similar to Gonorrhea, Salmonella can be easily prevented through the proper cooking and handling of poultry. Both resistant organisms also do have some sort of treatment, including combination therapy; however, the alarming rates of resistance must continue to be monitored and contained.
